Having been invited to be part of the early First Contact Practitioner (FCP) trials back in 2016, we have learned a huge amount about the ‘dos and don’ts’ of running an effective FCP service. Pure Physiotherapy now supports numerous Primary Care Networks across the country, with a clinically focused team of hundreds of FCP physiotherapists.
I am regularly contacted by Primary Care Networks (PCNs), clinical directors, and managers to discuss their FCP service and how improvements can be made. There are often three recurring themes that are consistent throughout the needs of the PCNs, and this has prompted me to share my experience and expertise in this series of blogs.
This blog will focus on introducing the three key themes that I believe are often the cause of an FCP service not performing to its true potential and could be deemed to be failing. In essence, these themes are engagement, training, and transparency and/or flexibility of the service.
I will aim to break these down into sections by context and narrative around each theme, as well as linking key actions to the governance structure outlined by NHS England.
The three key reasons why first contact practitioner services fail:
- Practices
- Patients
- Pathways
- Primary Care Networks
- Clinical experience (are your clinicians right for the role?)
- Support structure including the roadmap governance.
- Access to peer debriefing and CPD opportunities.
- Career development and feeling valued.
- Data collection
- How is the service performing?
- What are the outcomes?
- What do patients think of the service?
- What can we do better?
- Evolution of the service in a flexible way.
Poor engagement
Engaging people in any service is essential for its success. If someone does not understand the value of a service to themselves, then their willingness to be involved is negligible.
When reviewing services, I have been extremely worried about the lack of engagement that seems to take place in some FCP services, ultimately to its downfall. This undermines the entire service and often makes them ineffective and essentially pointless to the service users. Engagement needs to happen on multiple levels for FCP services to be successful.
Practices
Ensuring practice staff understand the FCP role, scope, and value that an FCP service can provide is key. All the members of a practice team play a vital role in making their FCP service successful. Engaging the practice team by providing training, ongoing education, and support is essential.
There is one group that stands out in the practices as being critical in making a successful FCP service. This group is not GPs, nurses, or practice managers (all of which are important), but it’s the care navigation team. The reception staff and the call handlers, who are the gatekeepers to booking and signposting patients, are key to ensuring the right patients are booked into the right service or clinician.
In the case of FCP physios, without a clear understanding of the benefits of an FCP appointment for patients with MSK issues, they are poorly equipped to book patients into the right clinical diary i.e., the FCP.
For example, the PCNs and practices we support at Pure Physiotherapy all have access to extensive reception and care navigation training during the mobilisation phase of a new service, but also (and importantly) on an ongoing basis.
Patients
Although FCPs have been embedded in many practices for years now, they are still relatively new to the primary care landscape. There are important and significant distinctions between a rehabilitation pathway physio service (typically in community or secondary care) and an FCP service in primary care. FCPs are there to prominently do two things:
- Reduce pressure on other front-line primary clinical staff for musculoskeletal (MSK) issues (up to 30% of primary care workload), and add value to patients in terms of management of their issues and effective outcomes.
- Setting expectations with patients is important to ensure that everyone involved gets the most benefit from the service. Essentially FCP physios are there as ‘MSK specialist practitioners’ in primary care.We are not there to provide a course of rehab or repeated treatment sessions; but to assess, safety net, educate, provide management plans, and organise appropriate workup or onward referral (where and when it is needed). Ideally, patients can rapidly access the service (within a few days) and we progress the patient’s care in an individualised and responsive way.
When engagement is not working then patients may attend expecting a course of massage, hands-on treatment sessions, or similar – and when this is not provided, they are dissatisfied. FCPs are there to integrate and help existing MSK pathways, not seek to duplicate or cannibalise them. Whilst we may not provide the full rehab pathway, we can refer to the local services.
Pathways
Similarly to the above, integration and engagement with existing local pathways are essential for a successful FCP service. This needs to be driven by both primary care and the existing local providers or pathways that serve patients.
I sadly hear about FCPs who are not making onward referrals, and everything goes back via a GP to make onward referrals, which duplicates the workload. This is not the intention of NHS England, and appropriately trained FCPs should be able to request imaging, carry out MSK injection therapy, and refer directly to local MSK and orthopaedic or rheumatology pathways.
I accept that the ability to demonstrate appropriate competencies is essential, and the cooperative working across primary and secondary care can occasionally have more friction than anyone would like. However, FCP offers a useful way of increasing the appropriateness of referrals into MSK pathways, reducing unnecessary imaging requests, reducing prescriptions for MSK issues, and improving conversion rates into surgical lists for those patients referred for a surgical opinion.
Primary Care Network (PCN)
Allowing an FCP service to be used equitably across a PCN is a good way for a PCN to show the constitute practices that the PCN is working for ‘THEM’ to improve services and reduce pressure. There are many ways in which FCPs can be structured and delivered to allow practices to benefit from the service across primary care network.
Whether that’s using a hub-based, physical, remote model, or a per head of population/per practice model – all can work well. Regardless of how you structure the FCP service, the engagement and collaborative working across the practices will help to ensure the best possible uptake of the FCP service.
Our organisation provides training and support through the service mobilisation process to all practices and the PCN management teams. This support is ongoing when a service is live, and I find this helps foster a collaborative and positive ethos across the organisations we support.
Poor staff training and support
Ensuring that the right level of health professionals move into first contact practitioner roles is key to the success of these services. Given the impact of these roles in primary care; the recruitment, training, and support of FCPs is paramount to creating an effective service to ensure clinical safety and effectiveness.
Clinical experience
Pure Physiotherapy now has a team of over 450 FCPs working across England. We recognise the critical importance of recruiting the right level of clinicians to move into FCP roles. There are substantial differences in the duties and roles of a physiotherapist working in a rehab pathway compared with a physiotherapist working in a first-contact role within primary care.
Setting the clarity around the role and what is to be expected, in terms of gaining the maximum impact for patients and practices is very important. This is often overlooked, and I can think of many examples where I’ve talked to PCNs who have a service or have directly recruited inexperienced physiotherapists, who are then unsure as to what the FCP role key targets are.
As a result of this, these physiotherapists tend to create more of a rehab physio service within primary care rather than the true first contact approach. Which in turn grossly limits the results in terms of patient benefits and reducing pressure on primary care staff. Even with experienced staff, clarity around the role and expectation is vitally important and requires setting out clearly, with regular reviewing as to outcomes and patient experience to ensure the service is running as it should.
Support structure including the roadmap governance
NHS England has produced a variety of governance road maps to ensure practitioners working in first contact roles have a clear structure. Ensuring they can demonstrate their clinical competence, to support patient and practitioner safety. In February 2022, the Care Quality Commission (CQC) stipulated and endorsed the need for all practitioners working in a first-contact role to evidence undertaking of these road maps. These are available on the landing page of the Health Education England website.
The long-term NHS plan published for primary care, which is due to be renewed in 2024, stipulates the requirement for time and encouragement to allow practitioners to undertake the road maps to practice. Over the last few years, I’ve come across multiple examples of organisations not allowing this time, or encouragement for the completion of clinical road maps. This has a twofold effect, firstly, adding significant clinical risk to both patients and practitioners; and secondly, jeopardising the CQC and governance safety structure of the individual practices, within which the physiotherapists are working.
Recruitment can be a challenge for many of the additional roles. Here at Pure Physiotherapy, we have a team of over 450 FCPs and reliably get over 3,000 applicants for FCP roles per month. This may seem a ridiculous figure and indeed it is, we have put systems in place to quality check and shortlist rigorously to ascertain the correct physios for FCP roles.
Many people who apply for these roles will be unsuitable to undertake the responsibilities, perhaps due to experience, skills, understanding of the role, previous experience in primary care, as well as understanding of the primary care landscape and NHS referral structures.
As a result of the 3,000 monthly applicants, we recruit between 10 and 20 new FCPs per month! It’s worth noting if you are looking at direct employment that our experience would indicate most people who are applying for these roles need very careful scrutiny before being offered a role in a First Contact Practitioner setting. Getting the right team members to support PCNs is important, getting the right level of physiotherapist for an FCP role is essential given the autonomous and independent clinical nature of the role.
Access to peer debriefing and CPD opportunities
The main goals of the ‘Road Maps to Practice’, published originally by Health Education England, now taken on by NHS England, are around ‘ensuring patient and practitioner safety.’ The road maps to practice focus on reflection, peer support, debriefing, training, and learning opportunities whilst in clinical practice. In discussions with FCPs and PCN leaders on courses that I teach on, one area that seems to have a huge discrepancy is the ability for FCPs to access regular peer support, which should ideally be daily.
We recognise this to be a key element required for a successful service; so back in 2016 we put in place structures to allow daily debriefs for any level of FCP regardless of experience, as well as a clinical helpline which is available from 7:30 am till 8:00 pm.
The helpline gives access to senior FCPs and Advanced Clinical Practitioners (ACPs) to discuss cases and come to a shared decision on patient management. This has been a cornerstone of how we deliver first contact physio. Having done this since 2016 (albeit not at that level of volume for the entire time), we have never had a negligence or clinical complaint.
The importance of regular peer-support debriefs and the ability to discuss cases with colleagues is critical. When FCPs struggle to access this support the risk to them as practitioners and to the patients they serve increases exponentially.
I am still surprised when I talk to an FCP, who is looking to join Pure Physio due to their experience of support, being wildly variable despite the clarity given by the road maps to practice. In some instances, physios will describe having access to discuss cases maybe once a week or even once a month. I have multiple examples where physios don’t feel able to discuss things with anyone in the work environment. This tends to make physios look to change roles or have issues with taking work home and become increasingly anxious about how they are performing from a safety and clinical effectiveness perspective.
I can’t stress enough that if you are to have a successful and sustainable first-contact service appropriate support structures for debriefing, peer support, etc. must be put in place and are adhered to.
Career development and feeling valued (patient feedback)
Since 2019 the introduction of FCP and other practitioner roles into primary care there has been a huge movement of experienced clinicians from rehab and secondary care pathways into primary care first contact roles. Understandably this has led to criticism around a ‘brain drain’ phenomenon affecting established rehab pathways. It has also meant that physiotherapists and other practitioners have moved into primary care, having perhaps not had a huge amount of experience in the specific focuses needed for effective primary care work.
Now that many of the first contact roles have been embedded into PCNs and practices, there is an increasing question about how people may progress or develop their careers. Many physiotherapists, for example, will look at injection therapy or independent prescribing as well as advanced clinical reasoning, which can help develop their skills within the role.
However, there is often no financial or career-level progression that can be made given the restrictions of the current NHS funding structure. This was improved by the lifting of the Advanced Clinical Practitioner threshold from one per PCN to several, and this may change again following the proposed changes in April 2024.
Many of the applicants we have for first contact roles within Pure Physio will cite their lack of career development and training opportunities to progress within the role as a key reason for them looking to join us. We are fortunate to be able to fund MSc and full PhDs, given our scale, and we are actively involved in the publication of research around MSK management in primary care.
I accept that this might be difficult to replicate this at an individual PCN level, but perhaps linking with GP federations, local training hubs, or multiple PCNs may allow each practice or PCN to offer a more long-term career plan for FCPs. The ability to see clear progression also helps to create a sense of being valued by the employer. At Pure Physio we add to this with the patient and line management feedback we give monthly to our team. I would encourage any PCN to look at providing regular feedback, not only from patients but from staff working within the PCN. This allows the FCPs to feel part of the team by having a sense of value in their role and seeing the opportunity to progress and develop within primary care.
Lack of transparency and flexibility
Being able to demonstrate the effectiveness of any service within healthcare is crucial to the viability of the service being offered. Given the relatively new creation of FCP, it’s arguably more important than ever that we collect appropriate data, feedback, and outcome information to evaluate its effectiveness. This information also aids understanding in how we can flex and evolve the services to meet patient demand for better outcomes.
Data and feedback
I am a huge advocate of collecting daily outcome data from patients, as well as feedback from practices and patients who use the service. Understanding what they found useful or effective from their treatment as well as what can be improved upon and changed. Unfortunately, when I discuss evaluating FCP services with Clinical Directors, PCN managers, and FCPs (who don’t work within Pure), I am amazed at the lack of consistent feedback and data collection occurring across the country.
There are of course some very good examples of PCNs and FCP providers collecting valuable data, feeding into research and providing that back to the PCNs to allow them to evolve services.
However, this is in my experience not the norm, with many PCNs not having good visibility or transparency in the way in which their patients are being managed. For example, a clear understanding of how many patients have accessed the service, as a genuine first point of contact, from a care navigator, reception staff member, or digital front door versus those referred internally after already having seen a GP or allied health professional.
To get the most effective first contact service we ideally want most patients referred to the FCP as their first clinical consultation. Once a patient has already been seen by one or two members within the primary care system before seeing a physiotherapist, we are not able to effectively reduce pressure on the practices or clinical staff as they’ve already taken up valuable appointment slots.
I believe the ability to collect data about how patients are accessing the service, and what outcomes are achieved following the consultation is extremely important. Whether that’s referral to secondary care, self-management, or any range of different options that are available to FCPs, a robust and consistent tracking of this information is vital, in my opinion.
Where a PCN has commissioned a third-party provider such as a trust, or an independent provider such as Pure Physiotherapy, to provide a supported first-contact service, I strongly believe it is the responsibility of that service to collect and provide the data back to the PCN; allowing them to make decisions based on transparent, honest feedback, and outcomes.
I recently discussed some challenges a PCN was having with their FCP service and was told that their DNA rate for FCP service was over 35% and had been at this level for some considerable time. I asked them what measures had been taken by the FCP organisation providing the service, and they were unable to answer. If you are commissioning a supported service you should expect; as the commissioning body, to receive support for that service.
It is my opinion this would include data collection, analysis of that data, and recommendations to implement positive change for the practices and patients that the service supports. In my experience, Pure Physio does not have any PCNS that have a DNA rate of over 10% or 11% at the absolute worst. Internally we have a flagging system that shows any DNA rate that tips over 10% in a month is then assessed and reviewed by a senior clinician and discussed with the PCN, to make sure it’s in line with current PCN services and doesn’t show a lack of engagement from patients.
By assessing and understanding data in a transparent way we can then proactively manage the service to deliver the best care for patients and reduce the maximum pressure on practices. There are many more examples I could mention around the value of meaningful data being provided to PCNs, which probably sits outside the scope of this blog. Come back soon to read my follow-up article…
Evolution and improvement of an FCP service
This data collection and analysis allows us to develop and evolve a service in an evidence-based way based on patient feedback and clinical outcomes. The last five years, since the NHS long-term primary care plan came into existence, has shown us the need to be flexible in the way in which we deliver healthcare to the populations we serve. The outbreak and impact of the COVID-19 pandemic had transformational effects on all GP practices across the country, and indeed the world.
This is a stark example of the need to have a flexible service within primary care, and FCP is not excluded from this. How a service is created needs to have the focus on practice pressures at the heart of it, and supporting the practices within a PCN in a flexible way will allow maximum patient and practice engagement and therefore the best possible service.
At Pure Physio we offer a range of service options, from traditional face-to-face FCP care to remote, whether that’s on a phone or video consultation – which is often favoured by PCNs where there is estate pressure. I would stress that a remote FCP service is only effective if key elements are being managed and often requires more experienced FCPs than you might normally expect to have in a face-to-face role, due to the additional complexity of remote-only working.
Most of the services we now support in primary care are face-to-face with an element of remote support perhaps to some of the more challenged estates practices. The need to flex between these two service delivery options and geographical locations across a PCN is important.
How we receive referrals and the training for the reception and care navigation teams needs also to be flexible based on the individual needs of the PCNs and practices. I come across multiple examples, particularly of PCNs we move to support from a previous provider, where very rigid referral criteria have been imposed upon practices. In some cases, they have been given quite stringent criteria to refer to a first contact service. I think many providers forget or are even ignorant of the fact that primary care networks and federations, and in some cases, individual practices, are commissioning this service and therefore it is incumbent on us as a service provider to flex to their needs, whilst adhering to the national governance structure of the FCP roles as outlined by NHS England.
I do believe one of the strengths and reasons that Pure Physiotherapy has managed to help support so many primary care networks is due to a combination of transparency, data in terms of quality and feedback, and flexibility to adapt to local needs in a positive and often proactive way.
Summary
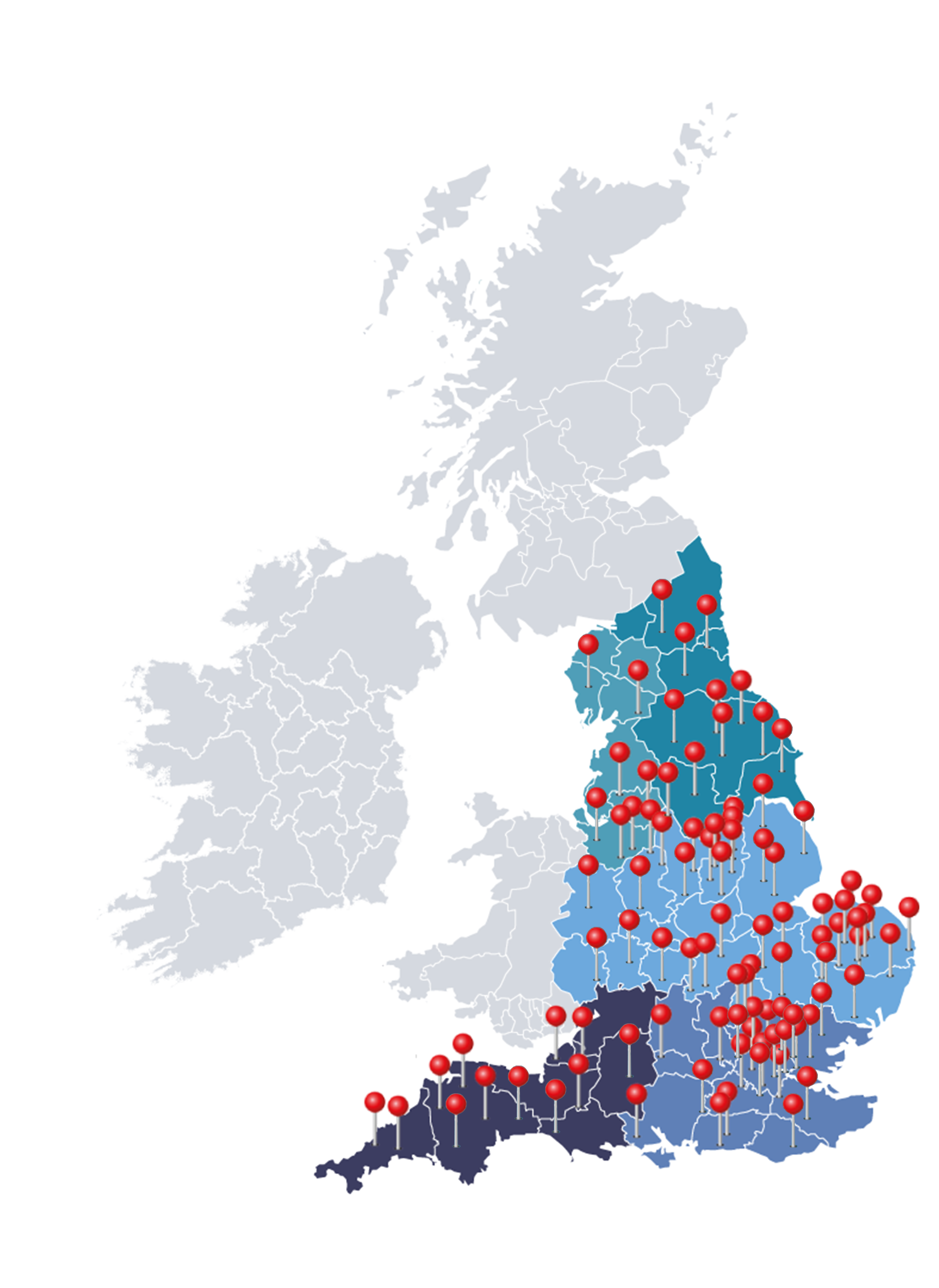
To summarise my experience since 2016, and the learnings we’ve gained by supporting over 220 PCNs with a large workforce of over 450 FCPs, is hard to do in a very concise way. However, there are recurring themes that I come across regularly which can struggle, and sometimes fail to deliver the quality consistency and impact that a well-run service can achieve.
The three key reasons why first contact practitioner services fail:
-
Poor engagement
-
Poor staff training and support
-
Lack of transparency and flexibility
I do believe that if we improve engagement with practices, patients, and PCNs, as well as the integration with local pathways – then you will see an improvement in the impact an FCP service can have and a reduction in the friction of a patient’s journey, from that first telephone call through to the conclusion of their episode of care.
To maintain patient and practitioner safety, as well as an enjoyable workplace within primary care for FCPs, providing the right level of training and support for FCPs is vitally important.
And finally, collect meaningful outcome data and patient feedback and use this to inform how you develop and evolve a service in a positive way in which you can maximise the benefit and increase the longevity of clinically useful services across primary care.
Author: Phin Robinson – Founder and Director, Pure Physiotherapy.