In this blog we explore the alternative models for utilising the Additional Roles Reimbursement Scheme funding (ARRS), which is currently being provided by NHS England until the 31st of March 2024. Following this date, it is understood that current ARRS funding will be wrapped into the core funding for PCN’s and GP practices. There has been a lot of discussion around this likelihood, and it is largely accepted that the ARRS funding level which is utilised in 2023-2024 will set the benchmark for the core funding, which will be allocated to PCN and practices following the end of the ARRS in 2024.
Our First Contact Physiotherapy (FCP) Experience
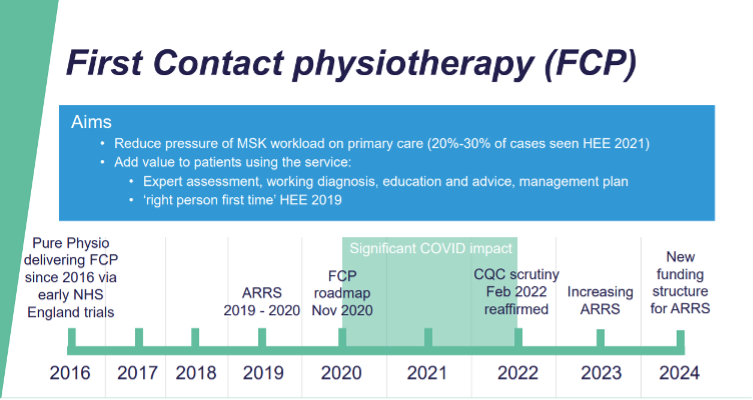
I have been working in primary care supporting musculoskeletal services since 2001 and head up a company called Pure Physiotherapy. We have been delivering direct musculoskeletal support for First Contact Physiotherapists since the early trials in 2016 supported by NHS England.
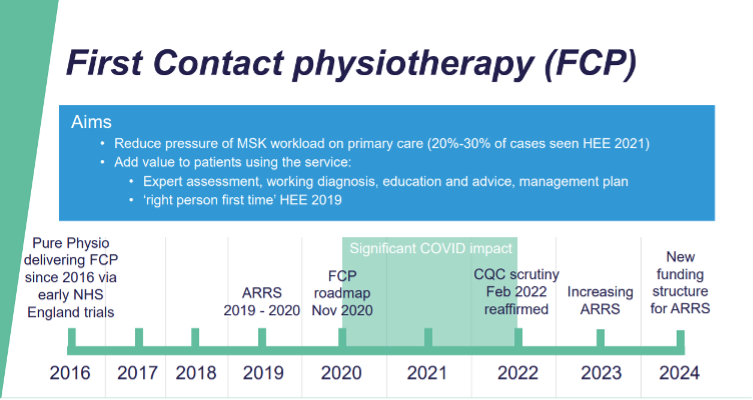
Part of my time is spent as an ambassador for the First Contact roles in primary care, and work for the National Health Education England team on delivering training to allow clinicians to sign off first contract practitioners as supervisors in primary care. We will draw upon that experience and link to NHS policy as well as elements around the recommendations from Health Education England around road map competencies and CQC requirements for practices utilising these roles.
The roles relating to the Additional Roles Reimbursement Scheme funding (ARRS)
The 17 roles which sit under the ARRS initiative are:
- Clinical pharmacists
- Pharmacy technicians
- The social prescribing link worker
- Health and well-being coaches
- Care co-ordinators
- Physician associates
- First contact physiotherapists
- Dieticians
- Podiatrists
- Occupational therapists
- Nurse Training Associates
- Nursing Associates
- Community Paramedics
- Advanced Practitioners
- General Practice Assistant
- Mental Health Practitioners (Adults and children)
- The Digital and Transformation Lead
These roles are designed to support primary care and patients served by primary care. Some of the roles are designed to be first-contact practitioner roles, which allows patients accessing primary care services to be seen in the first instance by certain healthcare professionals.
First contact physiotherapists are one of these roles and with the high frequency of patients attending primary care with musculoskeletal conditions, they are one of the more recognised roles for impacting and reducing workload on frontline primary care staff. Roles such as first contact paramedics, dieticians and others can also impact on direct frontline pressures.
ARRS Employment Models
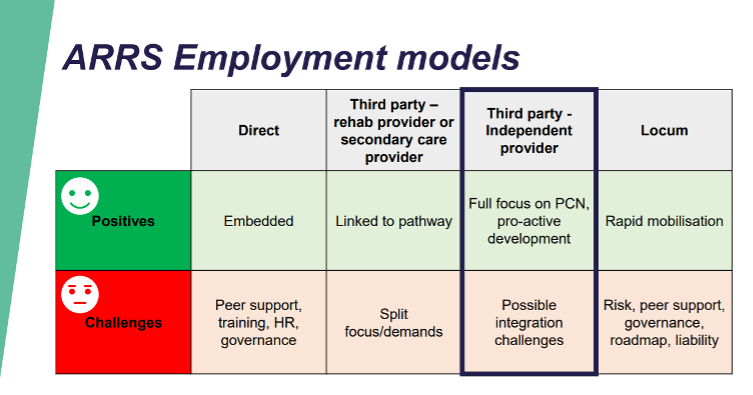
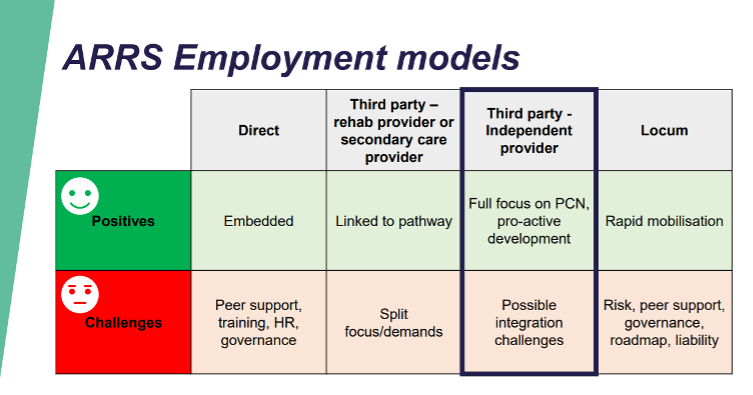
There are essentially three different routes to the employment of additional roles in primary care.
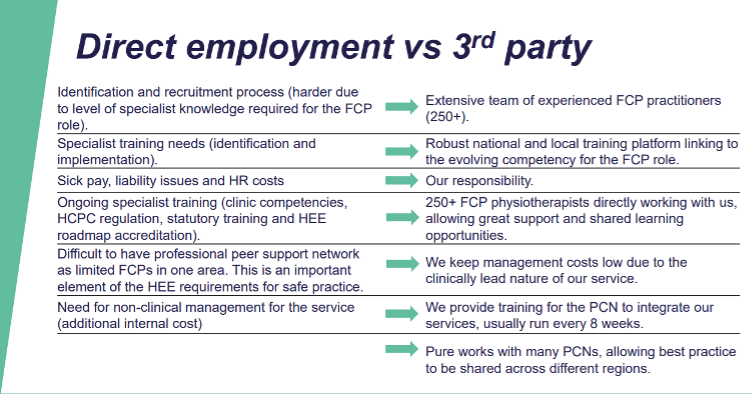
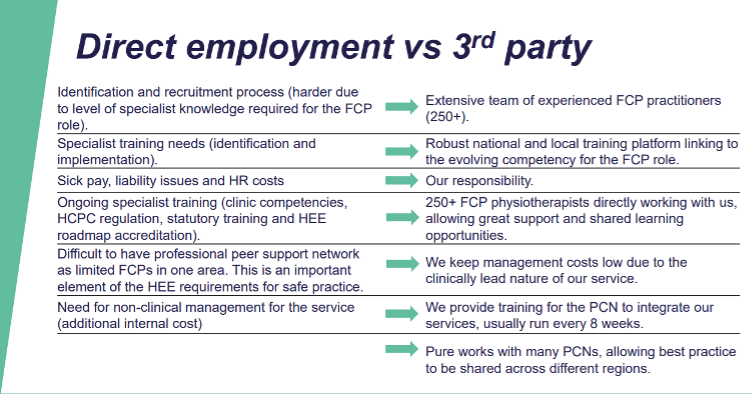
(1) A primary care network (PCN) can choose to directly employ an additional role
Whilst the benefits to this may include the ability to embed that member within the team, some of the challenges around support (if there are only one or two roles) within the PCN of a similar profession can be challenging. Within physiotherapy and other healthcare professions council regulated roles there are requirements for professional and clinical portfolios to be maintained, part of which is linked to peer support and professional development specific to the profession the individual is in. There are also additional costs to consider in terms of human resources, recruitment, mandatory training, IT training and ongoing support, as well as the clinical governance aspects for what could be a variety of different roles, which historically have not been managed directly in primary care.
(2) A PCN could choose to be supported by a third-party supplier
These suppliers could include an NHS Trust, rehabilitation pathway provider or an independent specialist provider. Pure Physiotherapy is a specialist provider of this nature giving PCNs fully supported first contact physiotherapists, who are compliant with appropriate regulations.
(a) if the third party provider was part of the rehabilitation pathway from secondary or community care, benefits can be seen as they are integrated within the local pathways; however, there can be challenges around the split focus of the FCP provider in primary care due to pressures in their core work leading to a split focus of their priorities, and in some cases pulling of first contact practitioners back into core service to support and manage waiting times and hospital based issues and challenges.
(b) An independent specialist provider such as Pure Physiotherapy is there to entirely focus on the PCN and practice needs, therefore rarely has split focus and is typically able to respond rapidly to changing needs of primary care.
(c) Effort is required by providers in this space to integrate with the community and secondary care services so there is no duplication and a patient’s pathway is as smooth and frictionless as possible. This does require time and effort on behalf of the FCP specialist provider and it would be incumbent on them to do this to ensure the healthcare system runs smoothly from primary to community to secondary care.
(d) At Pure Physiotherapy, we pride ourselves on collaborative working across these areas to ensure patients are triaged through appropriately, supporting onward pathways into community care and appropriate referrals for imaging and secondary care interventions as required. Essentially allowing a better triaging from a clinical perspective of patients moving into appropriate areas for their more specialist care as and if required.
(3) A locum-based model
There are significant risks with this approach given the issues around training, competency, governance, peer support and accountability. Even though the NHS road map was published several years ago and seeks to give some governance guidelines as to individuals undertaking FCP roles, an individual locum practitioner working with the PCN is likely to open that network and practice within which they work, to significant clinical risk and potentially CQC risk.
My advice would be to think very carefully if you are looking to take on any first contact practitioner role in a locum model and for safety, significant consideration would need to be given to how that individual will be supported, debriefed, regulated, and assessed as they progress with their time in your practice or PCN.
This is not an approach which I would ever recommend due to the high risk associated. Given the reiteration from NHS England that the additional roles in primary care should be considered a long-term option, ongoing contracts or employment should be considered for stability of patients and safety as well as allowing services to develop in a sustainable and progressive manner.
Considerations for deploying First Contact Practitioners into Primary Care
Having provided first contact practitioners into primary care since 2016 we have learnt there are several key elements which should be considered when looking at implementing a new role or service into primary care.
(1) Understanding the scope of the role
How that would potentially impact your patient population is fundamental to understanding the benefit of taking on such a service. For example, in a musculoskeletal setting it is largely understood that between 20% and 30% of the primary care workload will be musculoskeletal in nature, this is slightly increased in older demographics and slightly reduced in younger demographics.
Linking this to the knowledge that first contact physiotherapists specifically trained and accredited to assess and manage this, musculoskeletal pressure would allow PCNs and practices to recognise the value and therefore invest the time and effort in looking at developing a first contact physiotherapy service within their organisation
(2) Implementation
Once the need and demand has been assessed and the recognition of a first contact role in terms of that need being addressed has been analysed, then careful consideration is required to implement the service and integrate that into the existing services and processes within the GP practices. This detail is beyond the scope of today’s blog however, I will be writing a further blog on this topic as there are many variables. For example:
- do the GP clinics have appropriate estate space for face-to-face rooms to be available?
- Is the clinical hub on system one or EMIS module to allow booking from each practice into a shared diary?
- Is there a physical hub where patients would be prepared to travel away from each practice?
- Are there IT challenges across the practices with perhaps split clinical systems meaning more of a per practice model might be desirable?
All these elements will be explored in a future blog, although I’d be happy to discuss all of this with you personally. To get in touch, use the form below.
(3) Assessing the results
Once a service has been mobilised it is very important to be able to assess the impact. This assessment should take place in several way. For example, number of patients seen and utilization, onward referral and management to the patients within the service, types of patients seen and accessibility of the service, as well as DNA rates and potential issues which could create clinical risk.
The other crucial element to assess is the patient experience and feedback from individuals using the service. Health Education England published road maps to practice which are the governance structural recommendations for all first contact roles in primary care in England. Within these documents are stipulated patient feedback forms which each first contact practitioner should achieve 40 patient feedbacks per year as a minimum.
At Pure Physiotherapy, we aim to get between 200 and 400 patients to provide feedback each year. We use this to inform our services, put in place training and adapt where required, to maximize the patient benefit and therefore wider benefit to the practices in which we work.
“I have been given various excercises to improve my mobiltiy and I am feeling positive than an agred plan is in place for a successful recovery. Prior to this appointment I was feeling frustrated and didn’t know what to do the for the best”
(4) Respond to Patient Feedback
Utilising the data we gather as well as patient feedback should allow practices and PCNs to develop, adapt and improve their first contact services. We have certainly found the use of data and patient feedback crucial in how we have helped to support our staff to deliver the best possible service to the patients using the service.
The Impact of First Contact Practitioners
The additional roles in primary care can have a huge supportive impact on practices and patients. The first contact practitioner roles can arguably reduce pressure on frontline clinical staff such as GPs and nurses in a significant way. First contact physiotherapists can help manage up to 30% of primary care workload given the high level of musculoskeletal complaints attending primary care in England each year.
There are several ways of utilising first contact physiotherapists either directly employing or via a third party supported organisation. Locum type approach to first contact practitioners is not something I would endorse, and I do believe it is high risk and difficult to reconcile with patient safety, good clinical practice and development.
When considering implementing a first contact service, recognising the scope of the professional role, matching that to the demand and accessibility for patients within your particular primary organisation, and then planning a careful structured mobilisation and implementation plan is crucial. Following this, ongoing assessment through data and patient feedback should be promoted as a rolling program which can then be drawn from to develop and improve the service overtime.
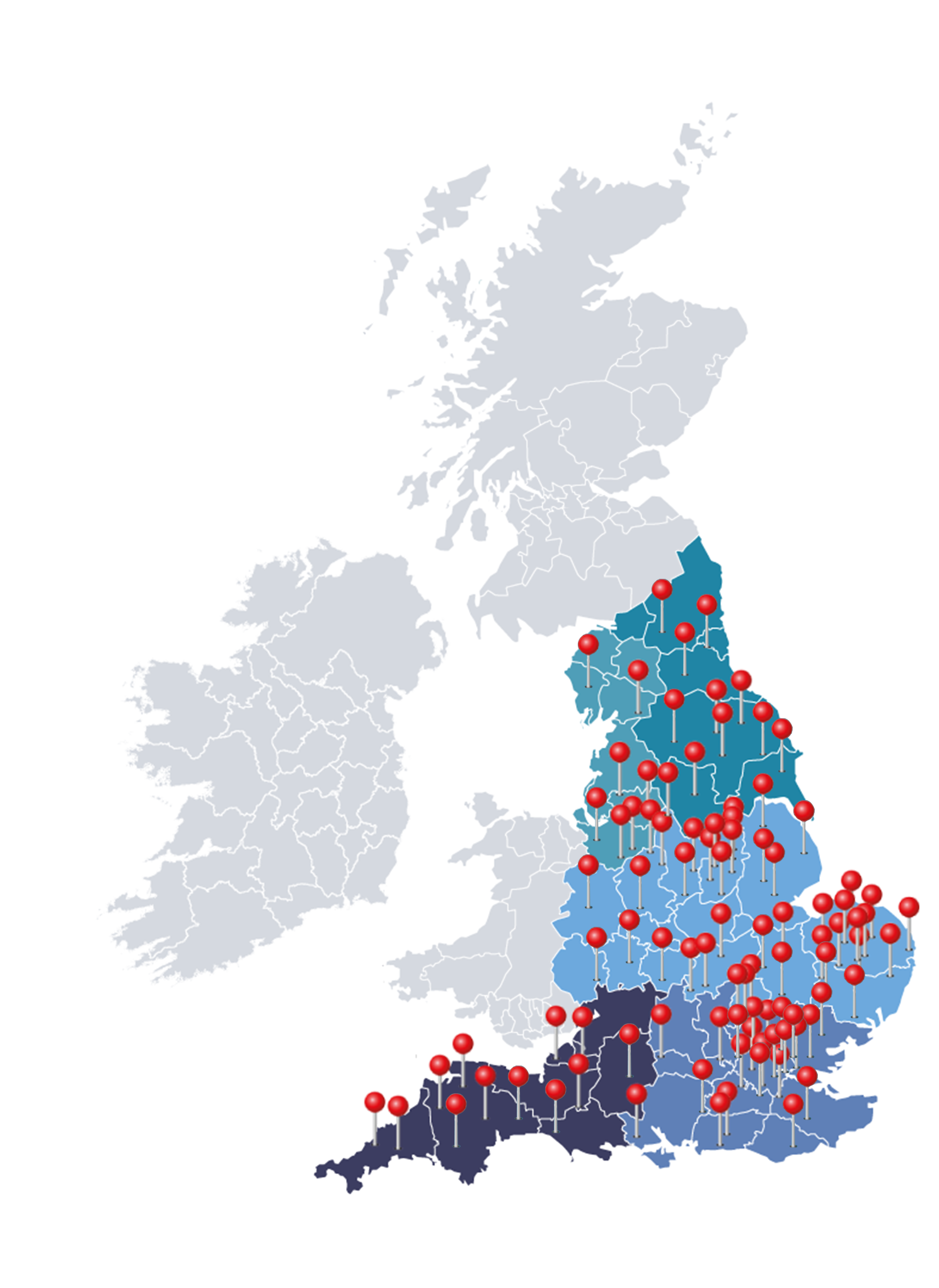
As someone who has worked in primary care for many years, I strongly believe that first contact roles within primary care can have a hugely positive impact. In Pure Physiotherapy alone we already see over 34,000 patients per month. We have managed to receive very good feedback from these patients as well as support their management in an evidence base and resilience building way.
One of the key elements with first contact physiotherapy is getting to see patients quickly, providing appropriate safety netting and then giving reassurance education and guidance to these individuals, who often link the pain they are feeling to a more catastrophic cause.
If you would like to discuss any elements of first contact physiotherapy or the wider roles added I would be more than happy to please use the form below.